
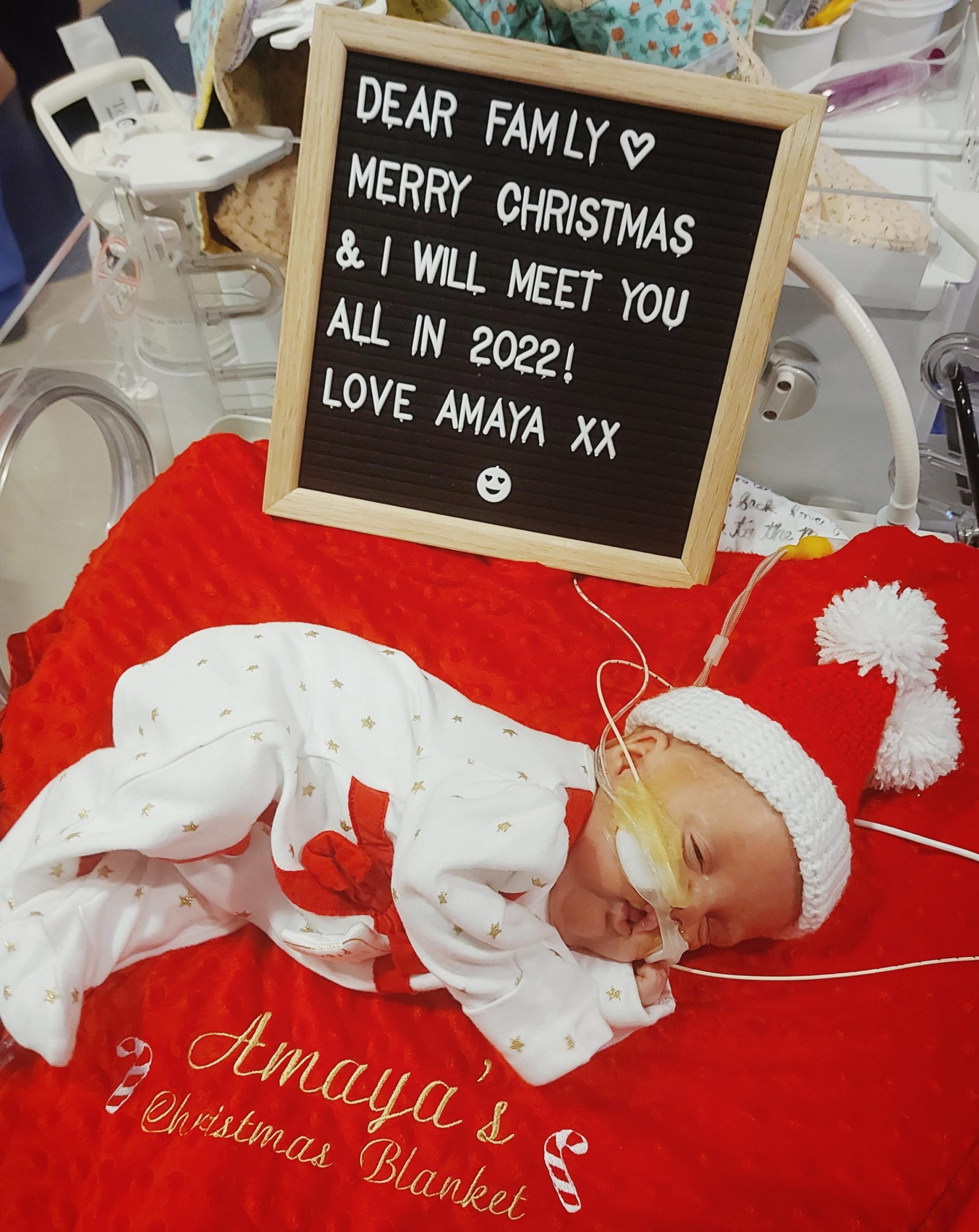
‘My miracle, my inspiration, my hero’: Amaya Rae’s story
December 19, 2022
Mischa was 23 weeks pregnant when she gave birth to her first baby, a little girl called Amaya Rae. Born on 28 August 2021 weighing just 680g, baby Amaya was immediately taken to the Neonatal Intensive Care Unit (NICU), where she was fighting for her life. Being born four months before her due date, Amaya’s parents were told she only had around a 20% chance of survival, her medical complexities including dangerously high potassium, brain bleeds, jaundice, and a lung haemorrhage.
She went on to being diagnosed with a rare heart condition, which has been treated with multiple surgeries and a clinical trial. During her lengthy stays in two different London hospitals, Amaya’s mum Mischa was accommodated in Ronald McDonald Houses, allowing her to spend as much time as possible with her daughter throughout a tumultuous first year of her life.

Guest blogger: Mischa
I had quite an easy pregnancy, other than the extreme tiredness and nausea. I was classed as ‘high risk’ due to an underactive thyroid, polycystic ovary syndrome (PCOS) and pelvic congestion syndrome (PCS) but the doctors didn’t have any concerns. Amaya’s scans were perfect, she was always very active. A couple of days before she was born, I was having cramps, and as the days went on, they were getting stronger and more frequent. I thought it must be Braxton hicks, and was not expecting to be in labour. I came home after a girls’ shopping trip one day and I had a ‘show’, and I instantly knew and felt that this was it and she was coming. I called for an ambulance, and they took me straight to the labour and delivery ward at East Surrey Hospital.
The doctor did his checks and just looked at me and said: ‘I am so sorry.’ There was no going back, my baby was coming. I was given steroids and magnesium and asked if I could try to avoid pushing for at least three hours, so the drugs could take effect. I was fully dilated at this point. The doctors were also trying to find a specialist neonatal intensive care unit (NICU). Nowhere had a bed for us and the risk of giving birth in transport was not a risk they were willing to take.
After three hours, they allowed me to push and within 10 minutes, Amaya Rae was born. The medical team took her away to work on stabilising her and the midwives worked on me. Once they got her ‘stable’, she was taken straight to NICU. My partner Jamie and I were left in a quiet room, with no baby and nothing but our thoughts. I felt empty, guilty, and angry. I couldn’t understand why my textbook pregnancy had led to having such a premature baby. I hadn’t heard her cry or been able to do skin to skin. Instead, I was left waiting, having been told the next 72 hours would be critical.

The first time I saw Amaya, was in a photograph taken by a midwife. I didn’t meet her until six hours later, so for a few long hours, all I had for comfort was a picture and an octopus toy that I could give to her so she could smell me. I thought I was fully prepared for what to expect when meeting her for the first time, but when I first walked into the NICU, I was surrounded by lots of babies, their parents, nurses, machines, and unfamiliar noises. It was a whole world that I didn’t really know existed, but this was my new world. The nurse walked over and said: ‘say hello to your baby, she is such a character already!’. She had been kicking and nibbling their fingers. When I first met her, my first thought was: ‘I am here now and we can do this together, no matter what’.

We waited for the transfer to take her to the Oliver Fisher Neonatal Unit at Medway Maritime Hospital. The travel incubator still haunts me to this day. How could this tiny little baby be moved into something that big? I held her tiny hand for the very first time whilst waiting for them to take her away again. I promised myself and Amaya that from that day on, I would hold her hand through every step, every trip, every milestone, and that’s exactly what I did and what I’m still doing.
Walking out of the hospital without my baby was one of the hardest things I’ve ever had to do. You feel completely empty and hopeless, like a part of you is missing. Whilst Amaya was being moved to a hospital in Kent, far away from home, we decided to go home first to refresh before another long day of the unknown.

When I walked through the double doors of the NICU unit in Amaya’s new ‘home’, I saw she was under blue lights to help with her jaundice. We soon discovered that the transport hadn’t gone well. During the journey, Amaya suffered a lung haemorrhage and a brain bleed. Little did we know that the complications of being a ‘micro preemie’ had only just begun.
On 14 September 2021, Amaya was transferred to Kings College Hospital London, where she had to have lifesaving surgery for spontaneous perforation of the bowel. Jamie and I missed her going down to the operating theatre, as we were travelling in from home and had to find an alternative route due to the eco protesters on the M25. It meant we had to give consent to the operation over the phone. Thankfully, her surgery went well; they removed 10cm of her bowel and created a stoma and mucous fistula.

Meanwhile, we were told about Ronald McDonald House Camberwell, which provides free accommodation to the families of children being treated at King’s. As soon as a room became available, we jumped at the chance of staying there. It was very daunting at first, moving into shared accommodation with lots of strangers but the staff were lovely and explained everything to us. The House was just a few minutes’ walk from the hospital, which meant I could spend more time with Amaya and less time travelling between the hospital and home. It saved us a lot of money in fuel and congestion zone charges and took away so much stress. Finally, I felt like I could breathe.

We ended up staying for seven-and-a-half months at the Camberwell House, while Amaya was admitted to Kings. That period was such a rollercoaster. As well as the major stomach surgery, she had hydrocephalus, multiple infections, blood transfusions and feeding issues. In October, she was transferred briefly to St Thomas’ Hospital for a surgical procedure to close her patent ductus arteriosus (PDA). She had to have eye injections for retinopathy of prematurity (ROP) and steroids to help strengthen her lungs. In December, she had her stoma reversed and came off the ventilator on her due date, 20 December. We felt like we were on the home stretch.
On 11 January, Amaya was moved from the intensive care unit (ICU) to the high dependency unit (HDU), which was a massive milestone, after 135 days in ICU. Discussions about moving her to a hospital closer to home began and things started to feel much more positive. However, the following month she had her vaccinations, and this is when took a turn for the worse. Her oxygen requirements were going up and an x-ray revealed she had fluid on her lungs. An echocardiogram showed she had pulmonary hypertension, which can be caused by having chronic lung disease. She was moved back onto ICU so the doctors could keep a close eye on her.

Not long after her move to ICU, Amaya went into respiratory distress which meant she needed to be ventilated. Before ventilating her, I held her in my arms, gave her the biggest cuddle and I just cried as my heart was breaking all over again, my greatest fear being that she would never be extubated. Once she was settled on sedation, another ‘echo’ was carried out, which confirmed she not only pulmonary hypertension but also pulmonary vein stenosis (PVS). PVS is a very rare heart condition where scar tissue builds up within the veins, making it difficult for the blood and oxygen to pump to and from the heart and lungs. A decision was made to send her to Evelina London Children’s Hospital, which has a specialist cardiac unit.

Moving hospitals meant a move for me from Ronald McDonald House Camberwell to Ronald McDonald House Evelina London, a much bigger accommodation facility offering the same type of brilliant support and allowing me to be moments’ away from my baby. My mum was also able to stay with us at the House. Having her there for support was invaluable, especially as we were about to face the worst news yet about Amaya’s health.

During a meeting with the cardiologist and the palliative care team to discuss her PVS, we were told the dreaded words: ‘I’m sorry, there’s nothing else we can do’. I felt numb and angry. To hear there’s nothing that can be done to save your child is possibly one of the worst things you can be told. The palliative care team told us she may only live for a few days and discussed end-of-life care options, either to take her home, stay in hospital or to go to a hospice. I wanted none of them.
The next day we were told that radiology noticed something on her CT scan and that the images had been sent off to Great Ormond Street Hospital (GOSH) for a second opinion. Once they got the report back the doctors had a meeting, and we were then told we had options. By some miracle, Amaya created a new pathway to enable the blood to flow from the top of the non-connected veins to the bottom. This is how she had managed to stay alive for so long.

The next important date for us was 21 February when Amaya went into the cath lab to have balloon dilation to expand her pulmonary veins. It was explained to us that this was only a temporary measure until she was big enough to have stents and that there was a strong chance she wouldn’t survive the procedure, either by going into a hypertension crisis or because her body wouldn’t cope with the anaesthetic.
The whole family came, family flew in from America, and family in Switzerland and Australia waited on tenterhooks for news. It was a long day, but as every hour ticked by with no news, we took that as good news. Five hours later I got the call to say Amaya had done well and was back from the lab. We could all finally breathe a little.

Two weeks after her balloon dilation, Amaya was transferred back to Kings and after 19 days of being ventilated, she finally came off the ventilator and we were able to hug her again.
On Monday 4 April, Amaya was taken back into the cath lab to stretch her pulmonary veins. The procedure wasn’t as long this time, but after the four-hour mark, I was dying to call them to see if they had any news, and they did – she had just come out and was doing well. Afterwards, they noticed on the x-ray that she was fighting a chest infection, so she had to remain in an induced coma for a few days to recover.
There was no let-up two months later when, in June, she contracted parainfluenza, which meant she had to have stents fitted in her heart to help improve blood flow and provide support. The cardiologist said that it was a balancing act between letting the virus take hold or enabling good heart function by putting stents in.

June wasn’t all bad, however, as we received a very special and unexpected visit from the former Duchess of Cambridge, Kate Middleton. I couldn’t believe that she found the time during the Queen’s Jubilee weekend, to come and visit staff, patients, and families in the hospital. It was so lovely of her. Although it was a private visit, Kate was happy to pose for a photograph with us, which is something Amaya and I will no doubt treasure for many years to come.

In August, we were able to take Amaya home to Crawley for a few days for her first birthday. I really wanted her home for that special milestone. Lots of family came over to celebrate and met her for the first time. Although it was amazing to be at home with her, it felt weird. She had to be brought home in an ambulance, as she was still on oxygen. We had an entourage outside waiting for her and the flat had been decorated for us. Amaya was fine, she didn’t bat an eyelid, but we felt really unsettled and had to keep checking she was still breathing. She was coming into our environment for the first time, after months of us being in her environment and it was all very strange.

Bringing her home properly, after her discharge, was a lot more relaxed. We finally made it home on 21 September after 360 days in hospital. There were times when I never thought she would make it home and I cannot count how many times she nearly died, and we needed to prepare for the worst. But keeping true to herself, she fought and proved everyone wrong. She will forever be my miracle, my inspiration, and my hero.

Being able to stay in the Ronald McDonald Houses throughout most of Amaya’s time in hospital, made such a difference. Having to travel back and forth from West Sussex to central London just wouldn’t have been viable for such a long period of time. Ronald McDonald House Charities UK made our lives so much easier. If something were to happen on the ward, we were just minutes away. I could just take a walk and go and see her. At Camberwell, in particular, the House enabled me to make friends with other NICU parents. I also appreciated the lovely staff in both Houses and at the Evelina London House, we were often treated to meals and takeaways paid for by the Royal Bank of Canada (RBC) volunteers who came to help every week.

My thanks also go to the amazing nurses and doctors who looked after Amaya for the first year of her life. My biggest thank you is to her cardiologist who didn’t give up on her. The future is still unknown, but Amaya is benefitting from being one of only two babies in the UK on an oral chemotherapy treatment trial, which it is hoped will prolong her life. But as a family we will treasure every milestone we have as, against the odds, we have been given a chance to have our baby home.

Help us provide free home away from home accommodation to support families with children in hospital with a donation.
